Former talk show host Wendy Williams has been diagnosed with aphasia and frontotemporal dementia, a progressive disorder that makes it difficult for a person to understand and express language, her team announced in a statement Thursday.
The 59-year-old was diagnosed with the disorders last year “after undergoing a battery of medical tests,” according to the statement.
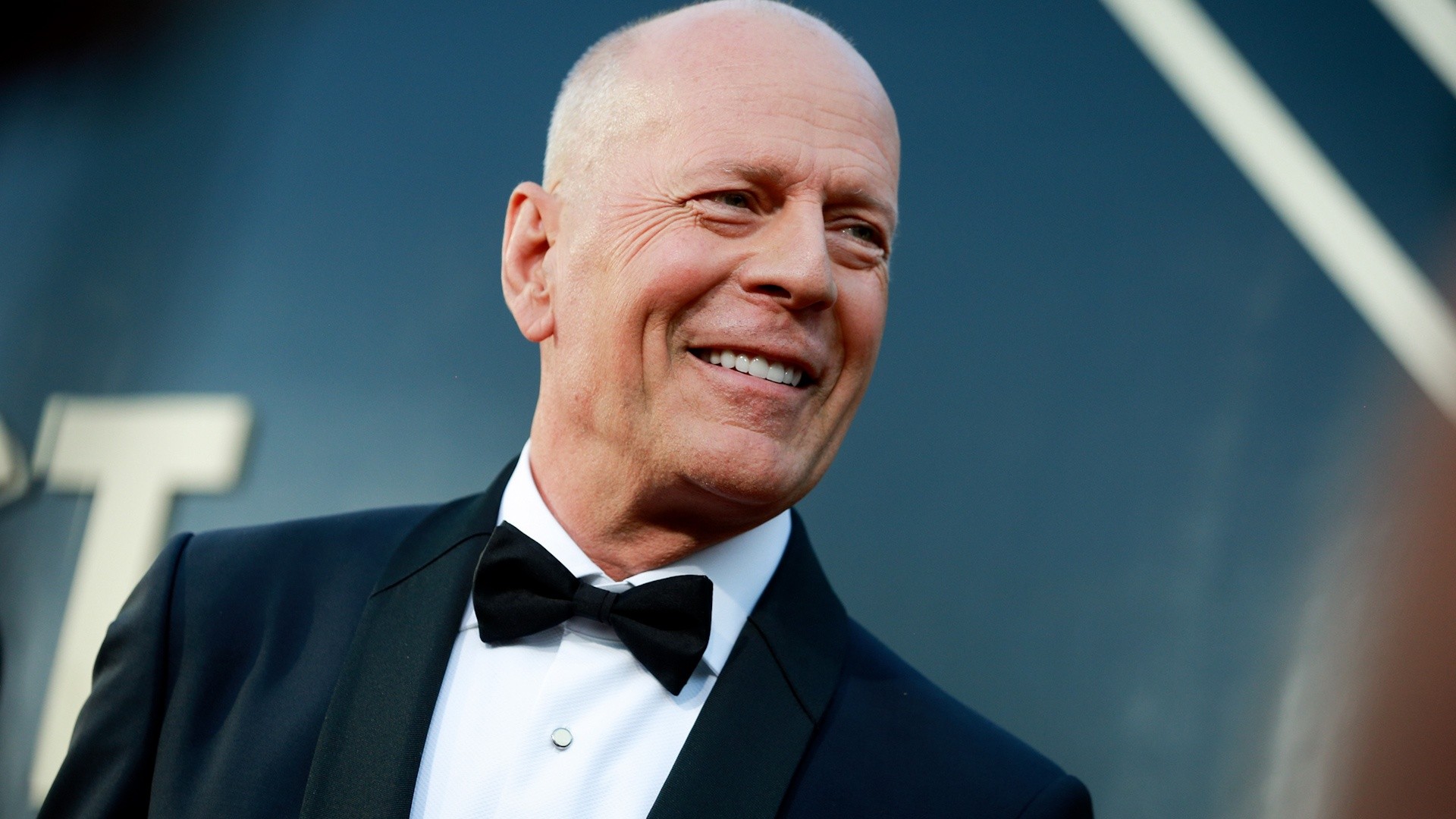
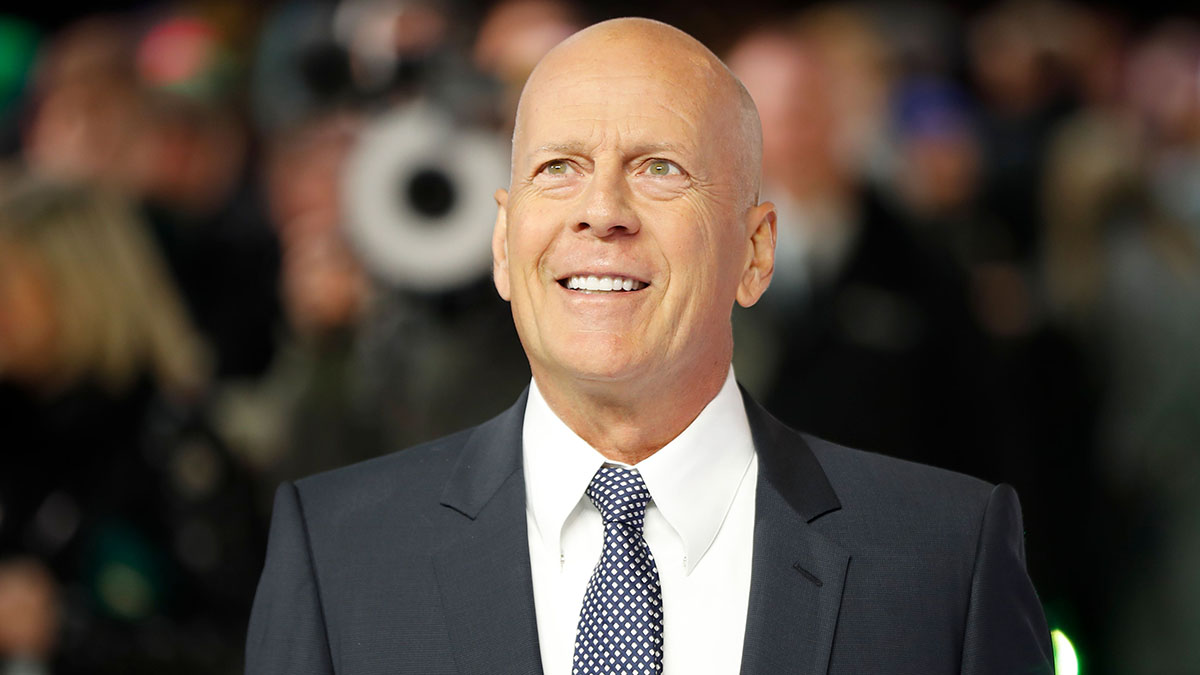
William's condition mirrors the same diagnosis given to actor Bruce Willis in 2022. The actor was diagnosed with Frontotemporal dementia late last year after initially receiving an aphasia diagnosis.
Frontotemporal dementia, or FTD, refers to a group of diseases that primarily affect the frontal and temporal lobes of the brain, the Mayo Clinic said. The disease often includes primary progressive aphasia, which means it’s causing problems with language skills.
What causes frontotemporal dementia?
The Mayo Clinic says several different diseases can cause frontotemporal degeneration but the two most prominent have to do with a group of brain disorders involving the protein Tau and a protein called TDP43.
FTD usually occurs in people in their 40s, 50s and early 60s. It can affect a person’s personality, causing a loss of inhibition or inappropriate behavior. It is sometimes mistaken for depression or bipolar disorder and can take years to diagnose.
In about a third of all cases, frontotemporal degeneration is inherited, the Mayo Clinic said. However, most people with FTD have no family history of it or other types of dementia.
Frontotemporal Dementia symptoms and diagnosis
Feeling out of the loop? We'll catch you up on the Chicago news you need to know. Sign up for the weekly> Chicago Catch-Up newsletter.
According to the Alzheimer's Association, the diagnosis of FTD starts with neurological exams, brain scans such as magnetic resonance imaging (MRI) and/or glucose positron emission scans.
Some of the first symptoms of FTD may include weight gain due to overeating, unusual or antisocial behavior, unusual verbal, physical, or sexual behavior as well as loss of speech or language.
In later stages, FTD patients can develop movement complications such as difficulty swallowing, muscle weakness, unsteadiness, rigidity, slowness or twitches.
What is the difference between Alzheimer's disease and FTD?
One of the biggest differences between Alzheimer's disease and FTD is that patients diagnosed with FTD generally exhibit personality disorders in the early stage, while memory decline often doesn't arise until the later stage.
In addition, Alzheimer's disease generally affects most areas of the brain, while FTD primarily affects the frontal and temporal lobes of the brain, which are the areas generally associated with personality and behavior.
How fast does FTD progress?
FTD can be a long illness, lasting two to 10 years. People with FTD will need caregiving or nursing support as their symptoms get worse.
“The disease will spread throughout the brain,” said Johns Hopkins University cognitive scientist Brenda Rapp. “The rate at which it does that is extremely unpredictable. So it’s very hard to know ... how quickly someone will deteriorate.”
The financial burden on families can be immense. The Alzheimer’s Association estimates it costs $10,000 a year, on average, for the out-of-pocket health and long-term care for a person with dementia.
Is there a cure for FTD?
The Alzheimer's Association says there are currently no specific treatments for any of the FTD subtypes.
There are, however, different medications that can reduce agitation, irritability, and/or depression. These treatments should be used to help improve quality of life but have not been proven to stop the disease.
"FTD inevitably gets worse over time and the speed of decline differs from person to person," the association said. "Individuals with frontotemporal dementia show muscle weakness and coordination problems, leaving them needing a wheelchair — or bedbound."
Some patients receive antidepressants or drugs for Parkinson’s, which has some overlapping symptoms with FTD. Genetic counseling and testing are also available in individuals with family histories of frontotemporal degeneration.