Warnings are increasing leading up to the holidays as cases of multiple respiratory viruses rise in the U.S. and in Illinois, but if you contract one, how long are you contagious?
RSV, COVID and flu activity were already on the rise for the state heading into the Thanksgiving holiday, leading health experts to urge caution. But things have only heightened from there.
But now, as of the week ending Dec. 9, nearly half of Illinois' 102 counties were at an elevated level of COVID-19 hospital admissions, according to CDC data.
Of the 48 counties at an elevated level, 10 are considered to be at a "high-level," meaning that they have recorded 20 or more COVID-19 hospitalizations per 100,000 people in the preceding week.
“As we celebrate this joyous time of year with our loved ones, it is important to know your personal risk factors for severe health outcomes and learn how to protect those around you, especially those most vulnerable to severe disease. COVID-19, flu, and RSV continue to circulate across Illinois, and I encourage all Illinoisans to use the many tools available to stay healthy and safe," Illinois Department of Public Health Director Dr. Sameer Vohra said.
The CDC last week took the unusual step of sending a health alert to U.S. doctors urging them to immunize their patients against the trio of viruses.
So, what if you are sick? How long are you contagious and what can you do?
Health & Wellness
Here's a look at what to know this holiday season:
COVID
Feeling out of the loop? We'll catch you up on the Chicago news you need to know. Sign up for the weekly Chicago Catch-Up newsletter.
Health officials are keeping an eye on a version of the ever-evolving coronavirus, known as JN.1. The omicron variant was first detected in the U.S. in September and now accounts for an estimated 20% of cases. The CDC expects it to reach 50% in the next two weeks, the CDC's Dr. Manisha Patel said.
It may spread easier or be better at evading our immune systems, but there is no evidence that the strain causes more severe disease than other recent variants, health officials say. And current evidence indicates vaccines and antiviral medications work against it.
Symptoms
If you do suspect you've contracted COVID, here are some symptoms you might experience:
- Cough
- Sore throat
- Runny nose
- Sneezing
- Fatigue
- Headache
- Muscle aches
- Altered sense of smell
Recently, a Chicago-area doctor said she's noticed shifts in the most common symptoms her patients have reported when contracting the COVID-19 virus this fall.
Dr. Chantel Tinfang, a family medicine physician with Sengstacke Health Center at Provident Hospital of Cook County, noted that many of the recent cases she's seen have reported less of the fever, body aches and chills, and more presented with sore throat, fatigue and coughing.
"We still see some patients experiencing decreased appetite, a loss of taste or smell. So it kind of depends," she said. "One patient was just very, very tired. Like she couldn't really do much. And that's when you know ... it's different. It's not just coughing and shortness of breath. We still see that though."
She suggested consulting with your doctor if your symptoms don't begin to improve outside of the recommended isolation period.
As for timing, symptoms can last for several days, but in some cases, even longer.
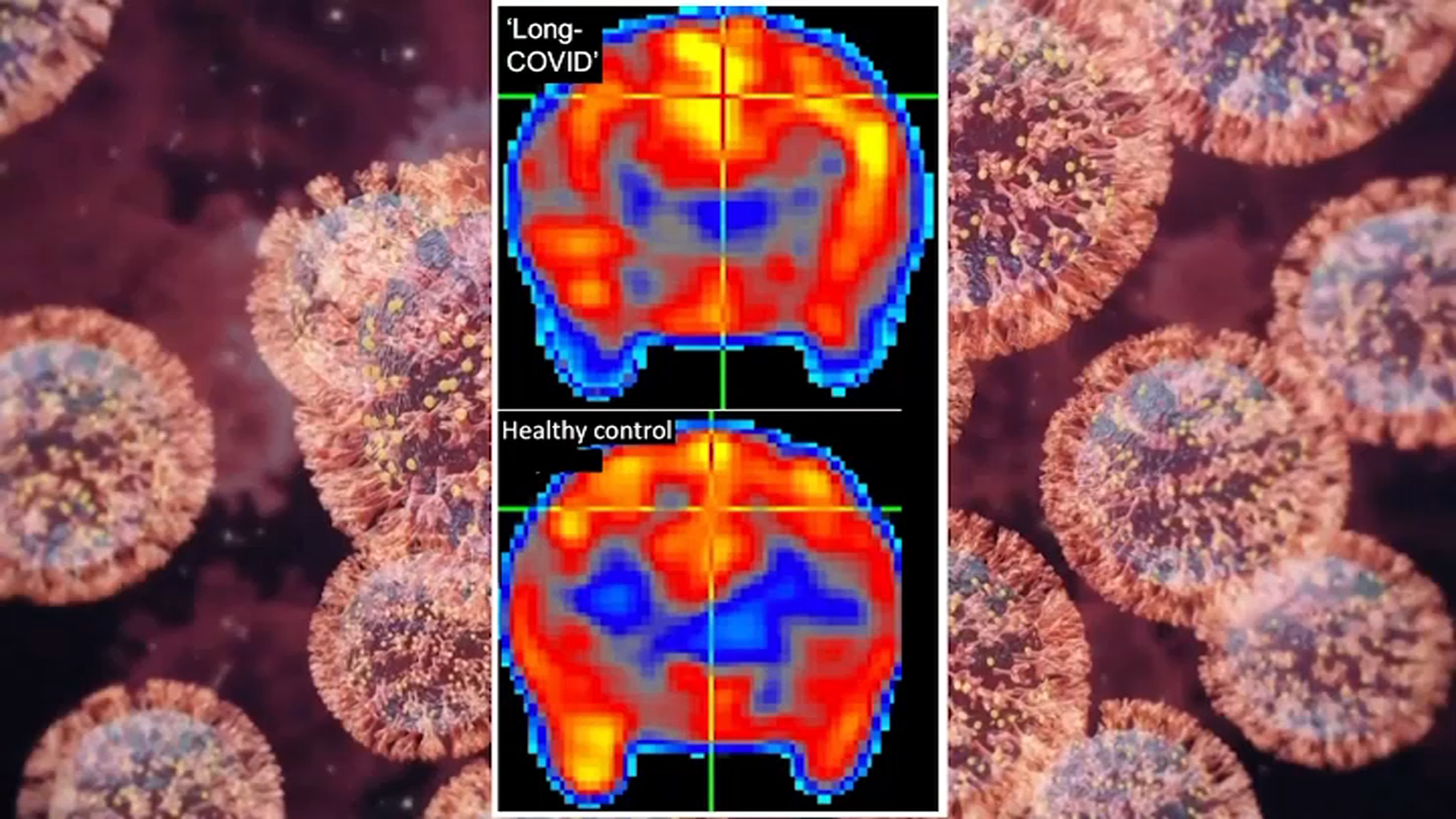
"Some people who have been infected with the virus that causes COVID-19 can experience long-term effects from their infection, known as Long COVID or Post-COVID Conditions (PCC)," according to the CDC.
Such symptoms can last for weeks and possibly even years.
Testing
In the lead-up to the holidays, the federal government has increased the number of free tests available for U.S. households.
That means all households are eligible to order up to four free at-home COVID tests, but those households that did not order them earlier this fall can receive up to eight, according to the government.
But when should you test and how often?
Those who have symptoms are urged to take a COVID test as soon as possible, though officials continue to caution that a negative at-home test may not be as reliable as a positive one.
"If your antigen test is negative, take another antigen test after 48 hours or take a PCR test as soon as you can," the CDC states.
Those who don't have symptoms but may have been exposed should wait five days after exposure to take a test, according to the CDC guidance.
Some experts say you could test even earlier, but most recommend to continue testing through day five if those tests are negative.
“I would say the best rule of thumb is to start testing three days after exposure, and if you’re negative, test again on day four or five,” Dr. Michael Mina, a COVID testing expert and former professor of epidemiology and of immunology and infectious diseases at the Harvard T.H. Chan School of Public Health, told NBC News.
PCR tests can also pick up lower levels of the virus and would offer a more accurate determination for those looking for one.
The steps for what to do if you test negative can depend on symptoms, however.
The FDA recommends symptomatic "people who get an initial negative result on an antigen test, take at least one more test 48 hours later."
"Take a third test, 48 hours after the second, if the second test was negative and you don’t have symptoms. Self-tests are more likely to detect the virus if you have symptoms," the guidance states.
You may also want to consider contacting a healthcare provider to check for additional tests for other illnesses.
The CDC recommends if you don't have symptoms and test negative at least five days from your exposure that you repeat the test again 48 hours after your first test.
"If both tests are negative, then repeat testing after another 48 hours for a total of three tests," the guidance states.
For those taking at-home tests, however, it's important to ensure your test hasn't expired.
The Food and Drug Administration has extended the expiration dates of many popular at-home test products, which means some such kits may still be safe to use, CNBC reports. You can check expiration dates for each brand using a page on the FDA's website.
Guidelines and Protocols
How long are you contagious?
The answer depends on several factors.
Regardless of vaccination status, you should isolate from others when you have COVID-19, the CDC reports. You should also isolate if you are sick and suspect that you have COVID-19 but do not yet have test results.
If you test positive for COVID-19, you should stay home for at least five days and isolate from others in your home. The CDC notes that people are "likely most infectious during these first five days."
When you have COVID-19, isolation is counted in days, as follows:
If you had no symptoms:
- Day 0 is the day you were tested (not the day you received your positive test result)
- Day 1 is the first full day following the day you were tested
- If you develop symptoms within 10 days of when you were tested, the clock restarts at day 0 on the day of symptom onset
If you had symptoms:
- Day 0 of isolation is the day of symptom onset, regardless of when you tested positive
- Day 1 is the first full day after the day your symptoms started
If you had no symptoms, you can end your isolation after day five, but for those who experience symptoms, that line might be different, the CDC notes.
Those who have mild symptoms can end isolation after day five if they are fever-free for 24 hours, without using fever-reducing medication, but those with more moderate or severe illnesses will need to wait until day 10.
Those who have mild symptoms that are not improving should also wait until those symptoms are improving and they are fever-free for 24 hours.
Those with more severe illness may also want to consult with their doctor before ending isolation and could need a viral test to end their isolation period.
Despite ending isolation, those who test positive should continue to avoid people and mask through at least day 11, according to the CDC guidelines.
Vaccines
In late summer, officials approved updated shots that have a single target, an omicron descendant named XBB.1.5. They replaced vaccines that targeted the original coronavirus strain and a much earlier omicron version. In September, the CDC recommended the new shots for everyone 6 months and older.
Americans have been urged to get different iterations of the vaccines for more than 2 and 1/2 years. This year, COVID-19 deaths and hospitalizations fell to lower levels than seen in the previous three years.
"Studies have consistently shown that COVID-19 vaccines lower the risk of getting symptomatic COVID-19 and improve protection against serious illness, hospitalization and death," IDPH said in a release. "New evidence is also emerging that it can protect you from long COVID and flu vaccines are also protective against heart disease."
RSV
Respiratory syncytial virus levels are on the rise in Illinois, but have not reached similar levels to those seen in 2022.
"This year we're starting to see an RSV surge," Dr. Julie Holland, the vice president for pediatric primary care with the Chicagoland Children’s Health Alliance and the head of general pediatrics for Advocate Children’s Hospital and Northshore University Health Systems, told NBC Chicago. "Now, this is a fairly typical time of year for us to start seeing RSV. Last year was a very unusual year in which we had a tremendous surge that started in about September. So it was early. It went much higher than normal, meaning a lot more cases. Our hospitals were full, our ICUs were full. So this year, we're really hoping that doesn't happen. But we are kind of in the beginning of what we would expect to see in a normal year with a normal surge. So fingers crossed that it doesn't get much worse."
Symptoms
Symptoms of RSV typically appear within 4-to-6 days after infection, according to the CDC. Those symptoms can include runny nose, coughing, sneezing, wheezing, fever and decrease in appetite.
Infants typically experience different symptoms, including irritability, decreased activity and breathing difficulties. Symptoms appear in stages, rather than all at once.
How Long Are You Contagious?
According to the CDC, "people infected with RSV are usually contagious for three to eight days and may become contagious a day or two before they start showing signs of illness."
The agency notes, however, that some infants or people with weakened immune systems can spread the virus even after their symptoms end, for as long as four weeks.
Vaccines and Treatment
Specifically, RSV vaccines are recommended for individuals who are 60 years of age or older, according to the Centers for Disease Control and Prevention. The vaccine is also recommended for pregnant women between weeks 32 and 36 of their pregnancy.
Finally, for children who contract RSV, a monoclonal antibody shot called nirsevimab is being recommended for infants under eight months and toddlers at high risk for serious side effects from the virus. Studies cited by the IDPH show a reduction in hospitalizations of up to 77% for those who are given the treatment.
And only 17% of adults 60 and older had received new shots against another respiratory virus. RSV, respiratory syncytial virus, is a common cause of mild coldlike symptoms but it can be dangerous for infants and older people.
Flu
Traditionally, the winter flu season ramps up in December or January. But it took off in October last year, and is making a November entrance this year.
Tracking during flu season relies in part on reports of people with flu-like symptoms who go to doctor's offices or hospitals; many people with the flu are not tested, so their infections aren’t lab-confirmed. COVID-19 and other respiratory viruses can sometimes muddy the picture.
Alicia Budd, who leads the CDC’s flu surveillance team, said several indicators are showing “continued increases” in flu.
There are different kinds of flu viruses, and the version that's been spreading the most so far this year usually leads to a lesser amount of hospitalizations and deaths in the elderly — the group on whom flu tends to take the largest toll.
So far this fall, the CDC estimates at least 780,000 flu illnesses, at least 8,000 hospitalizations and at least 490 flu-related deaths — including at least one child.
Symptoms
According to the CDC, symptoms of flu include:
- fever* or feeling feverish/chills (not everyone will experience a fever)
- cough
- sore throat
- runny or stuffy nose
- muscle or body aches
- headaches
- fatigue (tiredness)
- some people may have vomiting and diarrhea, though this is more common in children than adults.
In addition to the most common symptoms, the CDC also lists "warning signs" to watch for in both adults and children.
Those include:
In children
- Fast breathing or trouble breathing
- Bluish lips or face
- Ribs pulling in with each breath
- Chest pain
- Severe muscle pain (child refuses to walk)
- Dehydration (no urine for 8 hours, dry mouth, no tears when crying)
- Not alert or interacting when awake
- Seizures
- Fever above 104 degrees Fahrenheit that is not controlled by fever-reducing medicine
- In children younger than 12 weeks, any fever
- Fever or cough that improve but then return or worsen
- Worsening of chronic medical conditions
In adults
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest or abdomen
- Persistent dizziness, confusion, inability to arouse
- Seizures
- Not urinating
- Severe muscle pain
- Severe weakness or unsteadiness
- Fever or cough that improve but then return or worsen
- Worsening of chronic medical conditions
How Long Are You Contagious?
"People with flu are most contagious in the first three to four days after their illness begins," the CDC states. "Some otherwise healthy adults may be able to infect others beginning one day before symptoms develop and up to five to seven days after becoming sick."
Vaccines
As for flu, early signs suggest current vaccines are well-matched to the strain that is causing the most illnesses, and that strain usually doesn't cause as many deaths and hospitalizations as some other versions.
But the bad news is vaccinations are down this year, officials say. About 42% of U.S. adults had gotten flu shots by the first week of December, down from about 45% at the same time last year, according to the CDC.